What is obesity?
Obesity is currently considered the most serious public health problem of the 21st century.
Obesity is a medical condition characterised by an excessive accumulation of body fat which can lead to negative health effects with a consequent reduction in life expectancy.
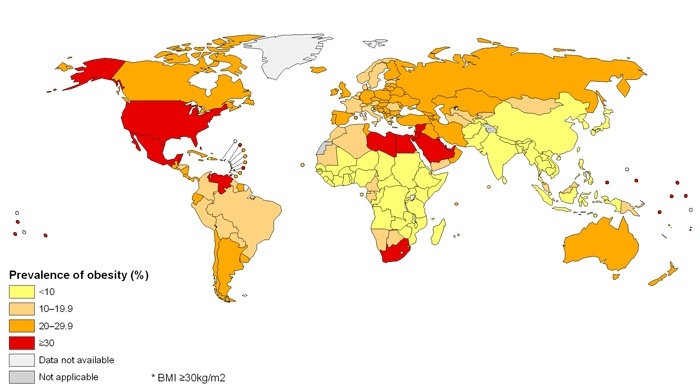
The world obesity map
How is obesity measured?

The World Health Association defines obesity using the Body Mass Index (BMI), a biometric figure which compares weight and height: those with a BMI of over 30 kg/m² are considered obese, while those with a BMI of between 25 and 30 kg/m² are considered overweight.
Patients with psoriasis are often overweight compared to the general population and are frequently obese. It is important for those with psoriasis to keep their body weight under control, because it can interfere with systemic treatment and reduce its efficacy.
The combination of weight loss, a balanced diet and physical exercise can contribute to reducing both relapses and the severity of the illness.
A history of psoriasis and diet

A study examined the effect of extreme dietary restrictions on psoriasis, such as those experienced during the First World War. During wartime, despite the obvious conditions of psychological stress, those with psoriasis and forced to adopt a limited diet showed an initial improvement in clinical symptoms, with a return of skin lesions after recommencing their previous diet.
Why is obesity a risk factor for psoriasis?

Numerous epidemiological studies have suggested that the clinical course of psoriasis may be influenced by a high BMI and obesity, as also suggested by their shared genetic aetiology.
Psoriasis and obesity share a number of pathogenic cytokines contained in visceral fat, including TNF-alpha, which as well as being elevated in psoriasis patches, play an important role in the pathogenesis of psoriasis.
TNF-alpha is also a marker of inflammation, and various anti TNF-alpha drugs are today used to treat moderate to severe psoriasis.
Various components of metabolic syndrome(which is not a single disease but a group of risk factors which increase the likelihood of developing cerebrovascular and cardiovascular diseases and diabetes) have been identified in psoriasis patients:
- an excess of body fat, especially in the abdominal area, known as visceral fat, leading to an increase in – weight/height ratio (BMI index)
- high levels of cholesterol and triglycerides in the blood
- high blood pressure (> 140/90)
- low levels of HDL cholesterol (“good” cholesterol)
- insulin resistance, with consequent hyperglycaemia
- hyperuricaemia

A review of the scientific literature has recently been published (Journal of American Academy of Dermatology) showing the clear link between metabolic syndrome and severe psoriasis.
Psoriasis does not only affect the skin, but is a “systemic” illness, which affects the whole body, and which is often associated with numerous other health problems.
The link between psoriasis and diabetes, obesity and BMI
 A Danish study, conducted on over 33 thousand twins and published in the scientific journal Jama Dermatology, demonstrates the link between psoriasis, diabetes, obesity and BMI. The Danish researchers analysed over 33,000 pairs of twins(aged between 20 and 71), 4.2% of whom suffered from psoriasis. After taking the subjects’ BMI into consideration, the researchers concluded that those with psoriasis were often overweight, particularly evident in the 720 pairs of twins in which one of the two siblings had psoriasis: those with patches on their skin was more often the twin who was overweight.
A Danish study, conducted on over 33 thousand twins and published in the scientific journal Jama Dermatology, demonstrates the link between psoriasis, diabetes, obesity and BMI. The Danish researchers analysed over 33,000 pairs of twins(aged between 20 and 71), 4.2% of whom suffered from psoriasis. After taking the subjects’ BMI into consideration, the researchers concluded that those with psoriasis were often overweight, particularly evident in the 720 pairs of twins in which one of the two siblings had psoriasis: those with patches on their skin was more often the twin who was overweight.
Another study conducted in 2014 by the Psoriasis Emilia Romagna Study Group involved 303 obese and overweight patients treated for 20 weeks with a diet plan and physical exercise.
The main outcome assessed by the research was a reduction in PASI score (indicating the severity and extension of the psoriasis), therefore a reduction in the extension of the area of psoriasis (of between 25 and 45%), as well as a reduction in the severity of the plaques, and above all a considerable increase in the efficacy of treatment.
The long-term impact of diet on psoriasis remains to be explored.
Conclusions
- Even minimal reductions in body weight can lead to significant improvements in response to treatment
- Reduction of treatment switches
- Reduction of costs
- Reduction of cardiovascular and metabolic syndrome risk factors